The Preoperative Evaluation
Key Points to Start:
*Remember, you can access Epic through the Ether website (ether.stanford.edu) whether on or off campus*
*If there is no Pre-op done in Epic, do a chart biopsy, look up old records, and call the patient (if necessary) to gather this important information that is vital in developing a safe and effective anesthetic plan*
*One question to always keep in mind while completing your pre-op: Is this patient optimized for surgery?*
Preop Templates
Check out these very cool preop template forms designed by Dr. Jared Pearson. I highly recommend you use them to notate your H&P and anesthetic plan for your cases.
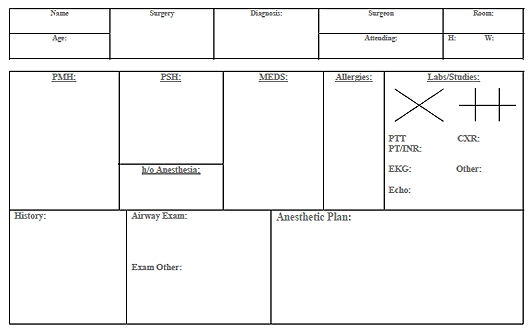 [Download PDF Version] [Download Word Document Version]
[Download PDF Version] [Download Word Document Version]
Dr. Chu and Dr. Harrison talk about and simulate the Preoperative Evaluation from March START podcast
Identifying Statement
- Name, age, sex, planned surgery and indication for procedure, surgeon
Past Medical History:
Remember to list all known medical history with specific emphasis on the following:
- Cardiovascular:
- Hypertension (baseline blood pressures, what medications, any complications)
- Coronary artery disease (hx of MI, stents/CABG hx, recent functional studies (stress testing, cath reports, echos)
- Arrhythmias (what medications used, any implanted devices, recent symptoms, Holter tests, etc)
- Pulmonary:
- COPD: (Medications used, frequency of exacerbations, steroid use, onhome oxygen, recent infections, any recent PFT information, recent CXR data ifapplicable)
- Asthma (Medications used, frequency of exacerbations, ever been intubated, steroid use)
- Smoking history (Pack year history, recent episodes of bronchitis, sputum production)
- Sleep apnea (may be a predictor of difficult airway)
- Gastrointestinal:
- GERD (Medications used, degree and frequency of symptoms)
- Inflammatory bowel disease (Steroids/immunomodulators used)
- History of post-operative nausea or vomiting
- Endocrine:
- Diabetes Mellitus (Type I vs II, medications used, home fingerstick readings, last Hgb A1C, any known macro/microvascular complications)
- Thyroid disorders
- Adrenal insufficiency
- Heme
- History of bleeding disorders, blood clots
- Is the patient on anticogulation medications? List any recent pertinent coagulation studies, if/when anticoagulation was reversed
- Neurological
- List any deficits including residual effects of old CVAs
- Rheumatological
- History of steroid use, lung/systemic involvement, any known joint (ie. atlanto-axial) instability
- **Looking at an old anesthetic record is crucial to see if there were any airway difficulties in patients with RA!**
- Pain
- Note preoperative pain score and document any history of chronic pain and list all preoperative pain medications and dosages taken by the patient (chronic opiate users may require more intra-operatively)
- Other
- List all other medical conditions
Review of Systems: Remember to be systematic and complete, with particular focus on the following:
- Constitutional: recent fevers or infections, nighttime sweating, motion sickness symptoms
- Cardiovascular: Exercise tolerance (how many stairs?), angina, activity level
*Patients who cannot meet the demand of 4-METS are high risk—Climbing a flight of stairs is 4-METs*
- Pulmonary: Shortness of breath, cough, dyspnea on exertion, smoker, use of inhalers, baseline oxygen if applicable
- Gastrointestinal: Reflux symptoms, NPO status
How long should your patient fast?
Solid food, milk, infant formula |
6 hours |
Breast milk |
4 hours |
Clear liquids (ie water, soda, juices, black coffee) |
2 hours |
*Any case which is emergent and these guidelines cannot be followed, rapid sequence intubation is indicated*
- Heme: Easy bruising or bleeding
- Musculoskeletal: Any cervical motion instability, myalgias, range of motion of extremities
Past Surgical History
- Past surgeries and their indications, any complications, where surgeries were performed (if known)
- Any implications for your plan? (ie cervical fusion surgery may impede normal intubation positioning)
Past Anesthetic History
- Prior history of adverse reactions to anesthesia, problems with airway management, difficult IV access, prolonged emergence, post-operative nausea/vomiting
*Prior anesthesia records are an invaluable source for this kind of information—find it and use it!!*
Risk Factors for Developing PONV
Procedure risks |
Patient risks |
Medication risks |
Laproscopic surgery |
Female |
Opioids |
Surgery on genitalia |
Non-smoker |
Volatile inhalation agents |
Craniotomies |
Prior PONV history |
Nitrous oxide |
Shoulder surgery |
History of motion sickness |
Neostigmine |
Middle ear surgery |
Young age |
|
Eye muscle surgery |
|
|
Family History
- History of malignant hyperthermia, pseudocholinesterase deficiency, or any other adverse reactions
Social History
- Alcohol use: How frequent, last drink, any complications from use
- Tobacco use: Duration in pack years, when patient last smoked
- Illicit drug use: Past or present use, when patient last used
- **Consider urine toxicology screen if clinically indicated to prevent autonomic instability**
Medications
- List all medications that the patient is taking, including over the counter and herbal medications. List the most important drugs first and give doses for important medication
- Especially medications for hypertension, diabetes, opiate pain medications, and blood thinners!
Allergies
- List all allergies, especially latex and antibiotics, and reactions to each allergen if known.
Preoperative Physical Examination
- Weight and height, vitals including room air saturation, and general appearance
- Airway: Includes Mallampati score, thyromental distance, cervical motion
Mallampati Scoring
Grade of View |
Structures Visualized |
1 |
Tonsillar pillars, soft palate, entire uvula |
2 |
Tonsillar pillars, soft palate, part of uvula |
3 |
Soft palate, base of uvula |
4 |
Hard palate only, no uvula visualized |
- Cardiovascular: complete exam with a focus on murmurs or rubs, check for bruits
- Respiratory: complete exam with a focus on wheezes or crackles
- Neurologic: complete exam, note any deficits discovered and compare to old records
- Extremities: complete exam, note any clubbing, deformities, bruising, and gauge level of difficulty for IV access
Additional Information
EKG
- Full interpretation including rate, rhythm, and ST changes. If available, compare to old EKGs to assess changes
Labs
- Review all recent labs and if abnormal results, compare to old values to assess changes
Assessment and Developing an Anesthetic Plan
ASA Status Classification
1 |
Healthy patient with no disease states |
|
2 |
Controlled medical conditions with mild systemic effects and no limitations in functional ability |
Controlled hypertension |
3 |
Severe systemic disease with limitations in functional ability |
Compensated CHF, stable COPD or angina, chronic renal insufficiency |
4 |
Poorly controlled/Severe systemic disease with significant functional impairment that is a threat to life |
Decompensated CHF, uncontrolled COPD, unstable angina |
5 |
Critical condition, death within 24 hours without surgery |
Ruptured AAA |
6 |
Brain dead |
Organ donor |
E |
Emergency |
Trauma, GI perforation |
Dr. Chu and Dr. Harrison model how to construct an anesthetic plan from March START podcast
- Consult the surgery listing to see how the surgeon booked the case—is this anesthetic option appropriate?
- Search resources in developing your plan
- Jaffe’s Anesthesiologist’s Manual of Surgical Procedures is an excellent pre/intra/post-op reference
- Consult your big sib or other colleagues to discuss your plan and inquire about other options
A talking point during your OR day could be developing your anesthetic plans for the following day’s cases!
- Define the type of anesthesia: MAC, GA, TIVA, Regional, etc
- Note what additional invasive monitors/IV access that will be required
Calling your Attending:
Dr. Chu and Dr. Harrison model how to call your attending to discuss your pre-ops from March START podcast
- You can find your Attending’s contact information here on ether, and click on “dashboard”
- Send courtesy page if no answer with short message (no patient information!) and callback number



